Heroin is a drug with intense side effects, and it can be difficult to know how long it will stay in your system if you’ve taken it. The answer to how long heroin stays in your system depends on a few factors, including how often you use the drug and how much you use.
This article will explore heroin, its side effects, how long it stays in your system, and how to get help if you’re struggling with addiction.
What Is Heroin?
Heroin is an illegal, highly addictive opioid drug. It is made from morphine, which is derived from the poppy plant.
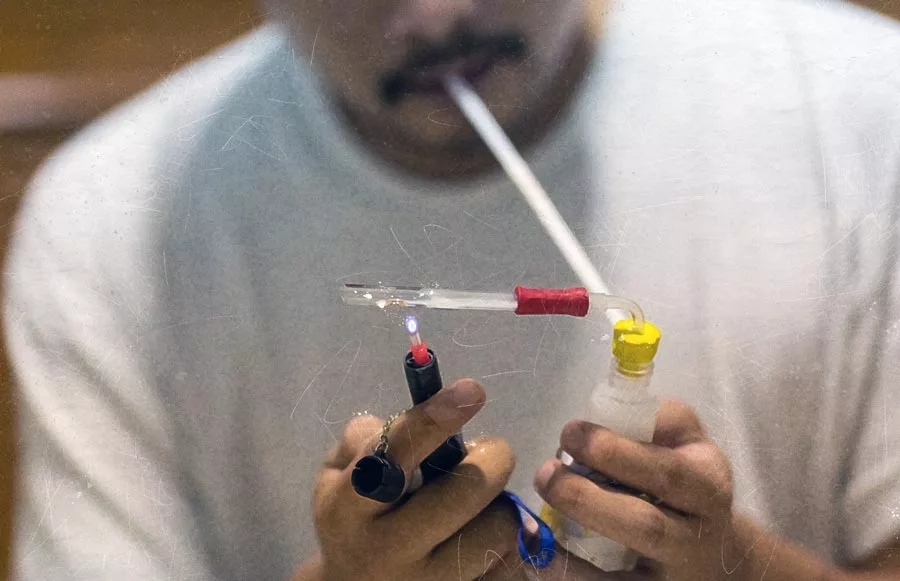
Heroin can be injected, snorted, or smoked, producing a powerful, short-lived high. The effects of heroin include a sense of euphoria, relaxation, and sedation.
The drug is highly addictive, and users can quickly develop a drug tolerance. Users will need to take larger doses to achieve the same effects with continued use.
Heroin use can lead to health problems such as collapsed veins, infection of the heart lining and valves, abscesses, and lung complications. It can also lead to psychological issues such as anxiety, depression, and insomnia, among others.
What Are the Effects of Heroin?
Heroin enters the brain quickly, producing a powerful rush of pleasure. It binds to the brain’s natural opioid receptors, which are involved in pain relief and feelings of pleasure.
It is one of the longest-acting and most potent opioids available, which is part of what makes it so addictive. The effects of heroin can last for four to six hours.
While the effect of heroin is long, it has a short half-life, which is the time it takes for half of the drug to be eliminated from the body. The half-life of heroin is only 30 to 90 minutes. This depends on how quickly the drug is metabolized and how much is taken.
How Long Does Heroin Stay in Your System?

When you are suffering from heroin addiction and desperately need help getting clean, drug tests may be required as part of the admissions process for some treatment programs.
The amount of time that heroin stays in your system depends on how often you use it and how much you use it.
Below are the factors that will affect how long heroin stays in your system:
- Frequency of use
- Drug quality (purity)
- Method of consumption
- Amount used
- Metabolism
- Weight
- Body fat percentage
- When you last used heroin
Generally, urine drug tests can detect heroin for around 24 hours after the last use. Blood tests and testing of hair follicles can be used to detect heroin for a more extended period.
Drug Testing Methods for Heroin
There are several types of drug tests, each with various detection windows.
1. Urine Test
Urine tests are the most common type of drug test. They are generally accurate and can detect most drugs for up to 24 hours after the last use.
For heroin, a urine test can detect the drug for up to 48 hours after the last use. Some urine tests can also detect heroin use and heroin metabolites for up to seven days.
2. Saliva Test
Saliva drug tests are one of the newest types of drug tests. Saliva tests are less invasive than urine or blood tests but are the least accurate.
A saliva test can detect heroin only 12 hours after the last use. Again, this depends on how much of the drug was used and how often it was used.
3. Blood Test

When you take a blood test, a small sample of your blood is drawn and sent to a laboratory for analysis. Blood tests are the most accurate type of drug test.
A blood test can detect heroin in your system for up to 24 to 72 hours after the last use.
4. Hair Follicle Test
A sample of hair near your scalp is taken and sent to a laboratory for analysis. Hair follicle tests can detect heroin use for up to 90 days, making it the longest-lasting drug test.
While this is the most accurate way to test for heroin use, it is also the most expensive.
How To Get Heroin Out of Your System
If you are trying to get the heroin out of your system, the best thing you can do is seek professional help.
Heroin is a highly addictive drug, and quitting cold turkey can be extremely difficult, if not impossible, on your own. Many different treatment options are available, and a professional treatment provider will help you choose the one that is best for you.
Sometimes, this may involve detoxification and rehabilitation in a hospital or treatment center. In other cases, it may be possible to find a less intensive outpatient program that can still provide the support you need.
Regardless of your path, getting professional help is the best way to increase your chances of success.
Best Rehabs In Arizonas are a leading provider of drug and alcohol abuse treatment. We offer a wide range of services, including detoxification, rehabilitation, and outpatient care. Our facility also provides various aftercare options to help you stay clean and sober after you leave our program.
Why Rehab is the Best Choice to Remove Heroin from Your System
Trying to get the heroin out of your system is extremely difficult if you have become dependent on the drug. Without professional help, the chances of success are very low.
For example, heroin withdrawal symptoms can be highly uncomfortable and even dangerous.
Below are some of the most common withdrawal symptoms:
- Nausea and vomiting
- Diarrhea
- Muscle aches and pains
- Fast pulse
- Increased breathing rate
- Sweating
- Anxiety
- Insomnia
- Irritability
These symptoms can make someone trying to quit using heroin feel very ill. Sometimes, they can lead to backsliding and relapse or hospitalization.
Heroin addiction treatment options are available in various settings, such as inpatient, outpatient, and partial hospitalization programs.
Licensed medical practitioners will help you through the detoxification process and make sure that you are comfortable and safe.
What is the Heroin Addiction Treatment Process?

Substance use disorder treatment usually follows these steps:
1. A Confidential Assessment for Substance Use
When you seek treatment for an addiction, the first step is always a thorough assessment. This allows the treatment team to get to know you and your unique situation. It also helps them develop a personalized treatment plan.
The assessment process usually includes reviewing your medical history, a physical examination, and a psychological evaluation. You will also be asked about your alcohol or drug use and your family history of substance abuse.
This information will help the treatment team determine what level of care you need and what type of treatment will be most effective for you. If you are ready to take the first step on the road to recovery, call us today. We can help you find the treatment that’s right for you.
2. Medically Supervised Detox for Heroin
Detoxification is the process of ridding your body of toxins, typically from alcohol or drugs.
The severity of detox symptoms depends on several factors, including how often you’ve been using, the type of substances you’ve been using, and your general health and well-being.
Detoxing without medical supervision can be dangerous, so it’s vital to be well-informed before embarking on the process. Some common detox symptoms include shaking, sweating, nausea, vomiting, and headaches.
For heroin, medications may be used to help with detoxes such as methadone or buprenorphine. These medications can help lessen withdrawal symptoms and make detox more tolerable.
If you’re considering detoxing, talk to a doctor or other medical professional first to ensure it’s the right decision.
3. Inpatient Rehab for a Foundation in Recovery
Rehabilitation is overcoming drug addiction and learning how to live a sober life.
During rehab, you will participate in individual and group therapy sessions. You will also have the opportunity to learn about addiction and recovery and how to manage triggers and cravings.
Inpatient rehab programs offer 24-hour supervision and care, which can be especially helpful during early recovery. These programs typically last 30 days, although more extended stays are sometimes necessary.
Outpatient rehab programs allow you to live at home while attending treatment during the day. These programs are less intensive than inpatient programs but can still be very effective.
4. Aftercare Planning and Relapse Prevention
Aftercare is any care you receive after completing a formal treatment program.
Aftercare can include 12-step meetings, therapy, and sober living houses. Aftercare aims to help you transition back into everyday life and maintain your sobriety.
While most clients will eventually graduate to self-sufficient recovery, some will require more ongoing care. This is often the case for clients with a dual diagnosis or those who have been through multiple treatment programs.
5 Things to Look for in a Heroin Addiction Treatment Program
A controlled substance like heroin can wreak havoc on your life, causing problems at work, in your home life, and your relationships. If you’re struggling with heroin addiction, there is hope.
Treatment can help you overcome addiction and learn how to live a sober life. But not all treatment programs are created equal. When looking for a treatment program, you should keep a few things in mind.
1. Individualized Care

One size does not fit all when it comes to addiction treatment. A good treatment program will offer individualized care that considers your unique situation.
This may include factors such as age, gender, the severity of your addiction, and any underlying mental health conditions.
In addition, the best treatment programs will also be flexible, offering different levels of care that can be adjusted to meet your changing needs. Tailoring treatment to your specific situation can increase your chances of achieving long-term sobriety.
2. Evidence-Based Treatment
When looking for a treatment program, you should ensure that it offers evidence-based treatment.
Evidence-based treatments are those that have been proven to be effective in scientific studies. These treatments are based on the latest research and are constantly refined to ensure they are as effective as possible.
Some common evidence-based treatments used in addiction treatment include cognitive-behavioral therapy, contingency management, and motivational enhancement therapy.
3. Fully Licensed and Accredited
You should also ensure that the treatment program you’re considering is fully licensed and accredited.
Licensing ensures that the program meets specific standards and is run by qualified staff. Accreditation shows that the program has been independently reviewed and found to be effective.
When you’re considering treatment programs, be sure to check that they are licensed and accredited. This will give you peace of mind that you’re choosing a program that is likely to be effective.
4. Comprehensive Services and Dual Diagnosis Programs
A good treatment program will offer a comprehensive range of services that address all aspects of addiction.
This may include detox, medication-assisted treatment, therapy, and aftercare. Those with dual diagnoses may also need additional services, such as psychiatric care.
By offering a comprehensive range of services, treatment programs can address all factors contributing to addiction.
5. Experienced and Qualified Staff
The staff at a treatment program can make a big difference in your recovery.
Look for a program that employs an experienced and qualified staff dedicated to helping you recover. The best staff will be compassionate, understanding, and firm in their commitment to helping you achieve sobriety.
With us, you will find a team of highly qualified and experienced staff who are devoted to helping you recover from addiction. Our staff includes doctors, nurses, therapists, and counselors committed to helping you achieve lasting sobriety.
If you’re looking for a heroin addiction treatment program that offers individualized, evidence-based care, look no further than our treatment center.
Further Resources on Heroin
If you’re looking for more information on heroin addiction treatment, here are some of the resources you may also want to check:
- Centers for Disease Control and Prevention (CDC): The CDC offers information on the risks of heroin use and how to prevent heroin addiction.
- National Institute on Drug Abuse (NIDA): NIDA is a government organization with helpful information on the latest heroin addiction and treatment research.
- Substance Abuse and Mental Health Services Administration (SAMHSA): SAMHSA is a government organization that offers resources on finding treatment for substance abuse disorders. They also have a helpline that can connect you with treatment providers in your area.
Forums and support groups like Narcotics Anonymous can help find treatment and support.
Our heroin addiction treatment program can help you achieve sobriety and live a healthy, happy life. Contact us today to learn more about our program or to schedule a consultation.
Find Your Path to Sobriety and Recovery Today
Drug tests are a reality of life for many people.
With heroin, how long it stays in your system depends on various factors, but generally speaking, it can be detected for up to 3 days in urine, up to 90 days in hair, and up to 14 days in blood.
If you’re concerned about drug testing, the best thing you can do is seek out treatment for your addiction. Contact Best Rehabs In Arizona Recovery now to help you get started on the road to a healthy life, without the worries of drug testing or being dopesick!